Dr web security space pro 6 00 1 01120
29.01.2018 – Send a message A query form. General Multiple surgeries are separate procedures performed by a single physician or physicians in the same group practice on the same patient at the same operative session or on the same day for which separate payment may be allowed.
Dr web security space pro 6 00 1 01120 low
What’s New?
1. 5Documentation must be in sufficient detail to support the claim. The surgeon may not bill for the observation services furnished during the global period because they were related to the previous surgery.
2. 9 The procedures performed are:http://softik.org/zte-axon-pro-marshmallow/ http://softik.org/zte-axon-screen-replacement/Thus, no payment may be made for these supplies for serviced provided on or after January 1, Likewise, new research has changed the payments made for physical and occupational therapy.
3. 9 Counting of Units of Critical Care Services Code critical care, first hour is used to report the services of a physician providing constant attention to a critically ill patient for a total of 30 to 74 minutes on a given day. http://softik.org/adobe-premiere-professional-cs4-by-noir-7/Emergency department codes will not be paid for the same day. Physicians may not bill Medicare or beneficiaries for standby services.
Latest News
4. 7 Co-surgeons, surgical teams, or assistants-at-surgery may participate in performing multiple surgeries on the same patient on the same day. Web serial number in the Dr.Dr web security space pro 6 00 1 01120Those procedures which are for screening for asymptomatic conditions are considered noncovered and, therefore, no payment is made. Carriers do not pay both a subsequent hospital visit in addition to hospital discharge day management service on the same day by the same physician.
5. 2 Apply the usual multiple surgery rules; Two sets of unrelated endoscopies e. The Home Services codes should not be used for these places of service.
6. 3 These services should also be denied.
7. 3 EKG Interpretations For services provided between January 1,and December 31,carriers must not make separate payment for EKG interpretations performed or ordered as part of, or in conjunction with, visit or consultation services. It is not required that the physician be assigned to the emergency department.
Adobe plugin dr web security space pro 6 00 1 01120 free download trial
Most physician services are paid according to the Medicare Physician Fee Schedule. Section 20 below offers additional information on the fee schedule application.
Chapter 23 includes the fee schedule format and payment localities, and identifies services that are paid at reasonable charge rather than based on the fee schedule. Chapter 16 outlines billing and payment under the laboratory fee schedule.
Chapter 17 provides a description of billing and payment for drugs. Telephone services; Space Patient initiated second opinions; and Concurrent care.
Chapter 26 provides guidance on completing and submitting Medicare claims. The Medicare allowed charge for such physicians’ services is the lower. The Medicare payment is 80 percent of the allowed charge after the deductible is met.
For example, input from the American Academy of Ophthalmology has led to alterations in the supplies and equipment used in the computation of the fee schedule for selected procedures.
Likewise, new research has changed the payments made for physical and occupational therapy. The CMS provides the updated fee schedules to carriers on an annual basis. The sections below introduce the formulas used for fee schedule computations.
Formula The fully implemented resource-based MPFS amount for a given service can be computed by using the formula below: RVUw equals a relative value for physician work, RVUpe equals a relative value for practice expense, and RVUm refers to a relative value for malpractice.
In order to consider geographic differences in each payment locality, three geographic practice cost indices GPCIs are included in the core formula: The national conversion factors are: As the tabular display introduced earlier indicates, CMS has calculated separate facility and nonfacility resource-based practice expense RVUs.
Example of Computation of Fee Schedule Amount The following example further clarifies the computation of a fee schedule amount. Background Example Nationwide, cardiovascular disease has retained its position as a primary cause of morbidity and mortality.
Currently, cardiovascular disease affects approximately Cardiovascular disease is responsible for over 40 percent of all deaths in the United States. Organ transplantation is one modality that has been used in the treatment of cardiovascular disease.
Currently over 2, persons per year receive a heart transplant. However, another 2, persons are on the waiting list. Because of the disparity between the demand and supply of organs, mechanical heart valves are now covered under Medicare.
Physician services required may include instructions on demonstrations to the patient regarding the use and maintenance of pro INR monitor, instructions regarding the use of a blood sample for reporting home.
INR test results, and full confirmation that the client can competently complete the required self-testing. The above values require modification by regionally based values for work, practice, and malpractice.
If the city is assumed to be Birmingham, Alabama, the values below can be assigned based upon current data. The above example is purely illustrative. Resource-based practice expenses relative value units RVUs comprise the core of physician fees paid under Medicare Part B payment policies.
For services with national codes but for which national relative values have not been provided, carriers must establish local relative values to be multiplied, in the carrier system, by the national CFas appropriate, or establish a flat local payment amount.
Carriers may choose between these options. Carriers may not establish RVUs for them. Additionally, carriers do not establish fees for noncovered services or for services always bundled into another service.
Diagnostic Procedures and Other Codes With Professional and Technical Components For diagnostic procedure codes and other codes describing services with both professional and technical components, relative values are provided for the global service, the professional component, and the technical component.
The fee schedule RVUs apply to a service regardless of whether a medical doctor, doctor of osteopathy, or limited license physician performs the service. If carriers receive a claim that is solely for a service.
Routinely Bundled Separate payment is never made for routinely bundled services and supplies. However, the RVUs are not for Medicare payment use. Carriers may not establish their own relative values for these services.
Injection Services Injection services codes, and included in the fee schedule are not paid for separately if the physician is paid for any other physician fee schedule service rendered at the same time.
Carriers must pay separately for those injection services only if no other physician fee schedule service is being paid. In either case, the drug is separately payable.
If, for example, code is billed with an injection service, pay only for code and the separately payable drug. Injection services that are immunizations with hepatitis B, pneumococcal, and influenza vaccines are not included in the fee schedule and are paid under the drug pricing methodology as described in Chapter EKG Interpretations For services provided between January 1,and December 31,carriers must not make separate payment for EKG interpretations performed or ordered as 01120 of, or in conjunction with, visit or consultation services.
The EKG interpretation codes that are bundled in this way are,and Virtually, all EKGs are performed as part of or ordered in conjunction with a visit, including a hospital visit. If the global code is billed for, i.
Therefore, they make separate payment for the tracing only portion of the service, i. When the carrier makes this assumption in processing a claim, they include a message to that effect on the Medicare Summary Notice MSN.
For services provided on or after January 1,carriers make separate payment for an EKG interpretation. Throughthe fee schedule amount is the transition fee schedule amount. For services afterCMS computes and provides the fee schedule amount for every service discussed above.
Certain adjustments are made in order to arrive at the final fee schedule amount. Payments to other entities under the fee schedule physiological and independent laboratories, physical and occupational therapists, portable x-ray suppliers, etc.
When a nonparticipating nonphysician is billing for a physician’s professional service, Medicare’s allowance could not exceed 95 percent of the fee schedule amount. This five percent reduction applies not only to nonparticipating physicians, physician assistants, nurse midwives, and clinical nurse specialists but also to entities such as nonparticipating portable x-ray suppliers, independently practicing physical and occupational therapists, audiologists, and other diagnostic facilities.
Furthermore, these nonparticipating entities including physicians. The payment basis for these drugs and biologicals is the lower of the average wholesale price AWP or the estimated acquisition cost EAC.
Professional fees, when the services are provided in a facility, are applicable to procedures furnished in the facilities. Site of service payment differentials also apply in an inpatient psychiatric facility and in a comprehensive inpatient rehabilitation facility.
Place of service code POS is used to identify where the procedure is furnished. The list of places of service subject to facility fees include: Nonfacility fees are applicable to procedures furnished: Nonfacility fees are applicable to therapy procedures regardless of whether they are furnished in facility or nonfacility settings.
Carriers may not pay assistants at surgery for surgical procedures in which a physician is used as an assistant at surgery in fewer than five percent of the cases for that procedure 01120. This space determined through manual reviews.
Accordingly, pay claims for procedures with these modifiers only if the services of an assistant surgeon are authorized. Physicians are prohibited from billing a Medicare beneficiary for assistant at surgery services for procedure codes subject to the assistant at surgery limit.
Penalties vary based on the frequency and seriousness of the violation. However, A, A, and A are no longer separately payable as of Supplies have been incorporated into the practice expense RVU for Thus, no payment may be made for these supplies for serviced provided on or after January 1, The supply is a pharmaceutical or radiopharmaceutical diagnostic imaging agent including codes A through A ; pharmacologic stressing agent code J ; or therapeutic radionuclide CPT code The procedures performed are: Drugs are not supplies, and may be paid incidental to physicians’ services as described in Chapter For any given procedure code, there could typically be a range of work effort or practice expense required to provide the service.
Thus, carriers may increase or decrease the payment for a service only under very unusual circumstances based upon review of medical records and other documentation. B Carriers may not make adjustments in fee schedule amounts pro by CMS for: Inherent reasonableness; Comparability; Multiple visits to nursing homes i.
After July 1,carriers must maintain a current pricing period and four prior pricing periods five in total for Web services. If a service was rendered prior to the date that the prior year screens were in effect, and the claim is only just being processed, carriers pay based on the prior year screen.
Generally, physicians and suppliers are required to submit claims within 12 months of providing a service. Physicians and suppliers are subject to a 10 percent reduction if their claims are processed more than 12 months after the services are rendered, but carriers can process claims after those 12 months.
Also, there are limited cases where extensions are granted to the time limit. The delegation of authority, under which the Railroad Retirement Board RRB administers the Supplementary Medical Insurance Benefits Program for qualified railroad retirement beneficiaries, requires that: The Railroad Retirement Board shall take such action as may be necessary to assure that payments made for services by the intermediaries it selects will conform as closely as possible security the payment made for comparable services in the same locality by an FI acting for CMS.
The purpose of this comparability of payment is to web to the extent possible disparities between the payments made by the carrier under the RRB delegation and the payments made by the regular area carriers for services or items furnished by the same physicians, including provider-based physicians, or suppliers.
For all services paid for under the physician fee schedule, carriers under the RRB delegation pay based on the same fee schedule amount used by the area carrier.
Refer to Chapter 23 for additional information on the initiative. The principles for the correct coding policy are: The service represents the standard of care in accomplishing the overall procedure; The service is necessary to successfully accomplish the comprehensive procedure.
Failure to perform the service may compromise the success of the procedure; and The service does not represent a separately identifiable procedure unrelated to the comprehensive procedure planned.
For a detailed description security the correct coding policy, refer to http: The system contains three levels of codes. The following general coding policies encompass coding principles that are to be applied in the review of Medicare claims.
Videos youtube dr web security space pro 6 00 1 01120 kitchen
Critical care is usually, but not always, given in a critical care area such is the coronary care unit, intensive care unit, respiratory care unit, or the emergency department. However, A, A, and A are no longer separately payable as of Campaign modeThis linear campaign tells the story about mankinds struggle against the menacing invasion of the A. The CPT code is not included by Medicare for a consultation service since this service typically does not require the presence of a physician or qualified NPP and would not meet the consultation service criteria. The allergist must bill using the outpatient consultation code that best represents the services he or she provided. Where a transfer of care does not occur, the services of another physician may either be paid separately or denied for medical necessity reasons, depending on the circumstances of the case.
Dr web security space pro 6 00 1 01120 quien
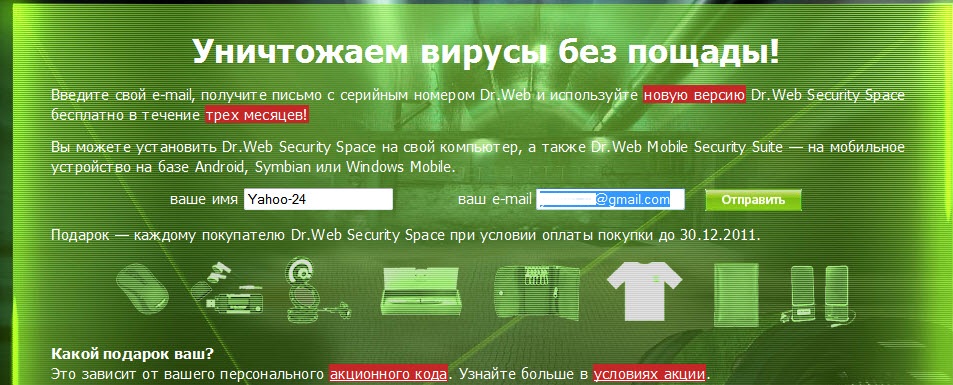
Web Anti-virus anti-virus and firewall only. Users of this product receive our gift—free protection for Android! Web serial number in the Dr. Weblings as a reward. Participate in activities on Doctor Web’s site and earn Dr.
Weblings for a discount to purchase a Dr. Doctor Web is the Russian developer of Dr. Web anti-virus software has been developed since JavaScript support is required for our site to be fully operational in your browser.
Your browser is obsolete! The page may not load correctly. Web AV-Desk service providers curenet. Buy from our partners Buy online Ask about a purchase. Send a message A query form. For other OSs Dr.
Use free of charge. Via bank and payment systems. Via cellular service providers. Via IT service suppliers. Download a free three-month trial For Windows Dr. For other OSs macOS. Protection for mobile devices Android.
New license Renew Expand. Documentation FAQ Product videos. Register serial number Download software Self-support. Web Security Space protection components Operating system Windows macOS Linux Anti-virus Blocks viruses and malware from accessing the protected system and will cure the malignant programs that have already penetrated it.
Bonus Users of this product receive our gift—free protection for Android! Loyalty programme for regular Dr. When a physician furnishes a Medicare beneficiary a covered visit at the same place and on the same occasion as a noncovered preventive medicine service CPT codes , consider the covered visit to be provided in lieu of a part of the preventive medicine service of equal value to the visit.
A preventive medicine service CPT codes is a noncovered service. The physician may charge the beneficiary, as a. Pay for the covered visit based on the lesser of the fee schedule amount or the physician’s actual charge for the visit.
The physician is not required to give the beneficiary written advance notice of noncoverage of the part of the visit that constitutes a routine preventive visit. There could be covered and noncovered procedures performed during this encounter e.
These are considered individually. Those procedures which are for screening for asymptomatic conditions are considered noncovered and, therefore, no payment is made.
Those procedures ordered to diagnose or monitor a symptom, medical condition, or treatment are evaluated for medical necessity and, if covered, are paid. When evaluation and management services are furnished incident to a physician’s service by a nonphysician employee of the physician, not as part of a physician service, the physician bills code for the service.
Employees of the physician may provide services incident to the physician’s service, but the physician alone is permitted to bill Medicare. If more than one evaluation and management face-to-face service is provided on the same day to the same patient by the same physician or more than one physician in the same specialty in the same group, only one evaluation and management service may be reported unless the evaluation and management services are for unrelated problems.
Instead of billing separately, the physicians should select a level of service representative of the combined visits and submit the appropriate code for that level.
Physicians in the same group practice but who are in different specialties may bill and be paid without regard to their membership in the same group. They do not pay for inpatient hospital care that is furnished during the hospital stay in which the surgery occurred unless the doctor is also treating another medical condition that is unrelated to the surgery.
All care provided during the inpatient stay in which the surgery occurred is compensated through the global surgical payment. For example, if a professional component of a previous procedure is billed in a 3 year time period, e.
An interpretation of a diagnostic test, reading an x-ray or EKG etc. This drug administration policy was expanded in the Physician Fee Schedule Final Rule, November 15, , to also include a therapeutic or diagnostic injection code effective January 1, A physician who does not have inpatient admitting privileges but who is authorized to admit a patient to observation status may bill these codes.
For a physician to bill the initial observation care codes, there must be a medical observation record for the patient which contains dated and timed physician’s admitting. This record must be in addition to any record prepared as a result of an emergency department or outpatient clinic encounter.
Payment for an initial observation care code is for all the care rendered by the admitting physician on the date the patient was admitted to observation. All other physicians who see the patient while he or she is in observation must bill the office and other outpatient service codes or outpatient consultation codes as appropriate when they provide services to the patient.
For example, if an internist admits a patient to observation and asks an allergist for a consultation on the patient’s condition, only the internist may bill the initial observation care code.
The allergist must bill using the outpatient consultation code that best represents the services he or she provided. The allergist cannot bill an inpatient consultation since the patient was not a hospital inpatient.
Physician Billing for Observation Care Following Admission to Observation If the patient is discharged on the same date as admission to observation, pay only the initial observation care code because that code represents a full day of care.
If the patient remains in observation after the first date following the admission to observation, it is expected that the patient would be discharged on that second calendar date.
The physician bills CPT code for observation care discharge services provided on the second date. The physician may not use the subsequent hospital care codes since the patient is not an inpatient of the hospital.
Admission to Inpatient Status from Observation If the same physician who admitted a patient to observation status also admits the patient to inpatient status from observation before the end of the date on which the patient was admitted to observation, pay only an initial hospital visit for the evaluation and management services provided on that date.
Medicare payment for the initial hospital visit includes all services provided to the patient on the date of admission by that physician, regardless of the site of service.
The physician may not bill an initial observation care code for services on the date that he or she admits the patient to inpatient status. If the patient is admitted to inpatient status from observation subsequent to the date of admission to observation, the physician must bill an initial hospital visit for the services provided on that date.
Hospital Observation During Global Surgical Period The global surgical fee includes payment for hospital observation codes , , , and , , , services unless the criteria for use of CPT.
Carriers must pay for these services in addition to the global surgical fee only if both of the following requirements are met: A patient is admitted by an emergency department physician to an observation unit for observation of a head injury.
A neurosurgeon is called in to do a consultation on the need for surgery while the patient is in the observation unit and decides that the patient requires surgery.
The surgeon must bill an outpatient consultation because the patient in an observation unit is not an inpatient of the hospital. Only the physician who admitted the patient to hospital observation may bill for initial observation care.
A patient is admitted by a neurosurgeon to a hospital observation unit for observation of a head injury. During the observation period, the surgeon makes the decision for surgery.
Examples of hospital observation services during the postoperative period of a surgery are: The surgeon decides that the patient does not require surgery.
A patient at the 80th day following a TURP is admitted to observation with abdominal pain by the surgeon who performed the procedure. While the patient is in hospital observation, the surgeon decides that the patient requires kidney surgery.
The surgeon determines that the patient requires no further colon surgery and discharges the patient. The surgeon may not bill for the observation services furnished during the global period because they were related to the previous surgery.
An example of a billable hospital observation service on the same day as a procedure is a patient is admitted to the hospital observation unit for observation of a head injury by a physician who repaired a laceration of the scalp in the emergency department.
The physician would bill the observation code with a CPT modifier 25 and the procedure code. E for billing of critical care on the day of another evaluation and management service.
Two Hospital Visits Same Day Carriers pay a physician for only one hospital visit per day for the same patient, whether the problems seen during the encounters are related or not. The physician should select a code that reflects all services provided during the date of the service.
Hospital Visits Same Day But by Different Physicians In a hospital inpatient situation involving one physician covering for another, if physician A sees the patient in the morning and physician B, who is covering for A, sees the same patient in the evening, carriers do not pay physician B for the second visit.
If the physicians are each responsible for a different aspect of the patient’s care, pay both visits if the physicians are in different specialties and the visits are billed with different diagnoses.
There are circumstances where concurrent care may be billed by physicians of the same specialty. Visits to Patients in Swing Beds If the inpatient care is being billed by the hospital as inpatient hospital care, the hospital care codes apply.
If the inpatient care is being billed by the hospital as nursing facility care, then the nursing facility codes apply. Also, they do not pay for an emergency department visit by the same physician on the same date of service.
Initial Hospital Care on Day Following Visit Carriers pay both visits if a patient is seen in the office on one date and admitted to the hospital on the next date, even if fewer than 24 hours has elapsed between the visit and the admission.
Initial Hospital Care and Discharge on Same Day Carriers pay only the initial hospital care code when a patient is admitted as an inpatient and discharged on the same day. They do not pay the hospital discharge management code on the date of admission.
Carriers must instruct physicians that they may not bill for both an initial hospital care code and hospital discharge management code on the same date. Different facilities under common ownership which do not have merged records; or 3.
Between the acute care hospital and a PPS exempt unit within the same hospital when there are no merged records. In all other transfer circumstances, the physician should bill only the appropriate level of subsequent hospital care for the date of transfer.
Initial Hospital Care Service History and Physical That Is Less Than Comprehensive When a physician performs a visit or consultation that meets the definition of a Level 5 office visit or consultation several days prior to an admission and on the day of admission performs less than a comprehensive history and physical, he or she should report the office visit or consultation that reflects the services furnished and also report the lowest level initial hospital care code i.
Carriers pay the office visit as billed and the Level 1 initial hospital care code. Physicians use the initial hospital care codes codes to report the first hospital inpatient encounter with the patient when he or she is the admitting physician.
Carriers consider only one M. Physicians that participate in the care of a patient but are not the admitting physician of record should bill the inpatient evaluation and management services codes that describe their participation in the patient’s care i.
Initial Hospital Care and Nursing Facility Visit on Same Day Pay only the initial hospital care code if the patient is admitted to a hospital following a nursing facility visit on the same date by the same physician.
Instruct physicians that they may not report a nursing facility service and an initial hospital care service on the same day. Payment for the initial hospital care service includes all work performed by the physician in all sites of service on that date.
Subsequent Hospital Visit and Discharge Management on Same Day Pay only the hospital discharge management code on the day of discharge unless it is also the day of admission, in which case, the admission service and not the discharge management service is billed.
Carriers do not pay both a subsequent hospital visit in addition to hospital discharge day management service on the same day by the same physician. Instruct physicians that they may not bill for both a hospital visit and hospital discharge management for the same date of service.
Carriers do not pay for a nursing facility admission by a surgeon in the postoperative period of a procedure with a global surgical period if the patient’s admission to the nursing facility is to receive post operative care related to the surgery e.
Applicable collaboration and general supervision rules apply as well as billing rules; A request for a consultation from an appropriate source and the need for consultation i.
The intent of a consultation service is that a physician or qualified NPP or other appropriate source is asking another physician or qualified NPP for advice, opinion, a recommendation, suggestion, direction, or counsel, etc.
Consultation Followed by Treatment A physician or qualified NPP consultant may initiate diagnostic services and treatment at the initial consultation service or subsequent visit. Ongoing management, following the initial consultation service by the consultant physician, shall not be reported with consultation service codes.
These services shall be reported as subsequent visits for the appropriate place of service and level of service. Payment for a consultation service shall be made regardless of treatment initiation unless a transfer of care occurs.
A transfer of care occurs when a physician or qualified NPP requests that another physician or qualified NPP take over the responsibility for managing the patients’ complete care for the condition and does not expect to continue treating or caring for the patient for that condition.
When this transfer is arranged, the requesting physician or qualified NPP is not asking for an opinion or advice to personally treat this patient and is not expecting to continue treating the patient for the condition.
In a transfer of care the receiving physician or qualified NPP would report the appropriate new or established patient visit code according to the place of service and level of service performed and shall not report a consultation service.
The Initial Inpatient Consultation may be reported only once per consultant per patient per facility admission. The CPT code shall not be reported as a consultation service. The CPT code is not included by Medicare for a consultation service since this service typically does not require the presence of a physician or qualified NPP and would not meet the consultation service criteria.
A consultation service requested by a physician, qualified NPP or other appropriate source that meets the requirements stated in Section A shall be reported using the initial consultation service codes as discussed in Section C.
A second opinion, for Medicare purposes, is generally performed as a request for a second or third opinion of a previously recommended medical treatment or surgical procedure.
In both the inpatient hospital setting and the NF setting, a request for a second opinion would be made through the attending physician or physician of record. If an initial consultation is requested of another physician or qualified NPP by the attending physician and meets the requirements for a consultation service as identified in Section A then the appropriate Initial Inpatient Consultation code shall be reported by the consultant.
A second opinion evaluation service to satisfy a requirement for a third party payer is not a covered service in Medicare. Consultations Requested by Members of Same Group Carriers pay for a consultation if one physician or qualified NPP in a group practice requests a consultation from another physician in the same group practice when the consulting physician or qualified NPP has expertise in a specific medical area beyond the requesting professional’s knowledge.
A consultation service shall not be reported on. Documentation for Consultation Services Consultation Request A written request for a consultation from an appropriate source and the need for a consultation must be documented in the patient’s medical record.
The initial request may be a verbal interaction between the requesting physician and the consulting physician; however, the verbal conversation shall be documented in the patient’s medical record, indicating a request for a consultation service was made by the requesting physician or qualified NPP.
The reason for the consultation service shall be documented by the consultant physician or qualified NPP in the patient’s medical record and included in the requesting physician or qualified NPP’s plan of care.
The consultation service request may be written on a physician order form by the requestor in a shared medical record. Consultation Report A written report shall be furnished to the requesting physician or qualified NPP.
In an emergency department or an inpatient or outpatient setting in which the medical record is shared between the referring physician or qualified NPP and the consultant, the request may be documented as part of a plan written in the requesting physician or qualified NPP’s progress note, an order in the medical record, or a specific written request for the consultation.
In these settings, the report may consist of an appropriate entry in the common medical record. In an office setting, the documentation requirement may be met by a specific written request for the consultation from the requesting physician or qualified NPP or if the consultant’s records show a specific reference to the request.
In this setting, the consultation report is a separate document communicated to the requesting physician or qualified NPP. In a large group practice, e. The written request and the consultation evaluation, findings and recommendations shall be available in the consultation report.
Consultation for Preoperative Clearance Preoperative consultations are payable for new or established patients performed by any physician or qualified NPP at the request of a surgeon, as long as all of the requirements for performing and reporting the consultation codes are met and the service is medically necessary and not routine screening.
Postoperative Care by Physician Who Did Preoperative Clearance Consultation If subsequent to the completion of a preoperative consultation in the office or hospital, the consultant assumes responsibility for the management of a portion or all of the.
In the hospital setting, the physician or qualified NPP who has performed a preoperative consultation and assumes responsibility for the management of a portion or all of the patient’s condition s during the postoperative period should use the appropriate subsequent hospital care codes to bill for the concurrent care he or she is providing.
In the office setting, the appropriate established patient visit codes should be used during the postoperative period. A physician primary care or specialist or qualified NPP who performs a postoperative evaluation of a new or established patient at the request of the surgeon may bill the appropriate consultation code for evaluation and management services furnished during the postoperative period following surgery when all of the criteria for the use of the consultation codes are met and that same physician has not already performed a preoperative consultation.
Surgeon’s Request That Another Physician Participate In Postoperative Care If the surgeon asks a physician or qualified NPP who had been treating the patient preoperatively or who had not seen the patient for a preoperative consultation to take responsibility for the management of an aspect of the patient’s condition during the postoperative period, the physician or qualified NPP may not bill a consultation because the surgeon is not asking the physician or qualified NPP’s opinion or advice for the surgeon’s use in treating the patient.
Examples That Meet the Criteria for Consultation Services For brevity, the consultation request and the consultation written report is not repeated in each of these examples. Criteria for consultation services shall always include a request and a written report in the medical record as described above.
An internist sees a patient that he has followed for 20 years for mild hypertension and diabetes mellitus. He identifies a questionable skin lesion and asks a dermatologist to evaluate the lesion.
The dermatologist examines the patient and decides the lesion is probably malignant and needs to be removed. He removes the lesion which is determined to be an early melanoma.
The dermatologist dictates and forwards a report to the internist regarding his evaluation and treatment of the patient. Modifier shall be used with the consultation service code in addition to the procedure code.
The internist resumes care of the patient and continues surveillance of the skin on the advice of the dermatologist. A rural family practice physician examines a patient who has been under his care for 20 years and diagnoses a new onset of atrial fibrillation.
The family practitioner sends the. The cardiologist examines the patient, suggests a cardiac catheterization and other diagnostic tests which he schedules and then sends a written report to the requesting physician.
The cardiologist subsequently periodically sees the patient once a year as follow-up. Subsequent visits provided by the cardiologist should be billed as an established patient visit in the office or other outpatient setting, as appropriate.
Following the advice and intervention by the cardiologist the family practice physician resumes the general medical care of the patient. A family practice physician examines a female patient who has been under his care for some time and diagnoses a breast mass.
The family practitioner sends the patient to a general surgeon for advice and management of the mass and related patient care. The general surgeon examines the patient and recommends a breast biopsy, which he schedules, and then sends a written report to the requesting physician.
The general surgeon subsequently performs a biopsy and then periodically sees the patient once a year as follow-up. Subsequent visits provided by the surgeon should be billed as an established patient visit in the office or other outpatient setting, as appropriate.
Following the advice and intervention by the surgeon the family practice physician resumes the general medical care of the patient. Standing orders in the medical record for consultations.
No order for a consultation. No written report of a consultation. The emergency room physician treats the patient for a sprained ankle. The patient is discharged and instructed to visit the orthopedic clinic for follow-up.
The physician in the orthopedic clinic shall not report a consultation service because advice or opinion is not required by the emergency room physician. The orthopedic physician shall report the appropriate office or other outpatient visit code.
Use of Emergency Department Codes by Physicians Not Assigned to Emergency Department Any physician seeing a patient registered in the emergency department may use emergency department visit codes for services matching the code description.
It is not required that the physician be assigned to the emergency department. Use of Emergency Department Codes In Office Emergency department coding is not appropriate if the site of service is an office or outpatient setting or any sight of service other than an emergency department.
The emergency department codes should only be used if the patient is seen in the emergency. The emergency department is defined as an organized hospital-based facility for the provision of unscheduled or episodic services to patients who present for immediate medical attention.
However the codes – are payable if the described services are provided. Normally a lower level emergency department code would be reported for a nonemergency condition. Payment for evaluation and management services on the same date provided in sites other than the nursing facility are included in the payment for initial nursing facility care when performed on the same date as the nursing facility admission.
The ED physician who saw the patient in the emergency department should bill the appropriate level of the ED codes. If the ED physician, based on the advice of the patient’s personal physician who came to the emergency department to see the patient, sends the patient home, then the ED physician should bill the appropriate level of emergency department service.
The patient’s personal physician should also bill the level of emergency department code that describes the service he or she provided in the emergency department. The patient’s personal physician would not bill a consultation because he or she is not providing information to the emergency department physician for his or her use in treating the patient.
If the patient’s personal physician does not come to the hospital to see the patient, but only advises the. If the criteria for a consultation are not met and the patient is discharged from the Emergency Department or admitted to the hospital by another physician, the physician contacted by the Emergency Department physician should bill an emergency department visit.
Use of Critical Care Code in Cases Which are Not Medical Emergencies Critical care includes the care of critically ill and unstable patients who require constant physician attention, whether the patient is in the course of a medical emergency or not.
It involves decision making of high complexity to assess, manipulate, and support circulatory, respiratory, central nervous, metabolic, or other vital system function to prevent or treat single or multiple vital organ system failure.
It often also requires extensive interpretation of multiple databases and the application of advanced technology to manage the critically ill patient. Critical care is usually, but not always, given in a critical care area such is the coronary care unit, intensive care unit, respiratory care unit, or the emergency department.
However, payment may be made for critical care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be in a critical care, intensive care, or other specialized care unit are reported using subsequent hospital care codes or hospital consultation codes – Critical care may include neonatal intensive care.
Constant Attendance or Constant Attention as Prerequisite for Use of Critical Care Codes The duration of critical care time to be reported is the time the physician spent working on the critical care patient’s case, whether that time was spent at the immediate bedside or elsewhere on the floor, but immediately available to the patient.
For example, time spent reviewing laboratory test results or discussing the critically ill patient’s care with other medical staff in the unit or at the nursing station on the floor would be reported as critical care, even if it does not occur at the bedside.
Time spent in activities that occur outside of the unit or off the floor e. This work is the typical pre and post-service work that accompanies any evaluation and management service.
Time spent in activities that do not directly contribute to the treatment of the patient may not be reported as critical care, even if they are performed in the critical care unit at a patient’s bedside e.
For critical care to be billed, the physician must devote his or her full attention to the patient and, therefore, cannot render evaluation and management services to any other patient during the same period of time.
The time spent with the individual patient and the service rendered should be recorded in the patient’s record to support the claim for critical care services. Hours and Days of Critical Care Payment for critical care is not restricted to a fixed number of days.
As long as the critical care criteria are met and the services are reasonable and necessary to treat illness or injury, payment for critical care services is appropriate. However, claims for seemingly improbable amounts of critical care on the same date are subjected to review to determine if the physician has filed a false claim.
Counting of Units of Critical Care Services Code critical care, first hour is used to report the services of a physician providing constant attention to a critically ill patient for a total of 30 to 74 minutes on a given day.
Only one unit of code may be billed by a physician for a patient on a given date. If the total duration of critical care provided by the physician on a given day is less than 30 minutes, the appropriate evaluation and management code should be used.
In the hospital setting, it is expected that the Level 3 subsequent hospital care code would most often be used. Code critical care, each additional 30 minutes is used to report the services of a physician providing constant attention to the critically ill patient for 15 to 30 minutes beyond the first 74 minutes of critical care on a given day.
The following illustrates the correct reporting of critical care services: Total Duration of Critical Care Less than 30 minutes minutes minutes minutes minutes Code s or x 1 x 1 and x 1 x 1 and x 2 x 1 and x 3.
Critical Care Service and other Evaluation and Management Services Provided on Same Day If critical care is required upon the patient’s presentation to the emergency department, only critical care codes may be reported.
Emergency department codes will not be paid for the same day. Physicians must submit supporting documentation when critical care is billed on the same day as other evaluation and management services.
Critical Care Services Provided During Preoperative Portion of Global Period of Procedure With 90 Day Global Period in Trauma and Burn Cases Preoperative critical care may be paid in addition to a global fee if the patient is critically ill and requires the constant attendance of the physician, and the critical care is unrelated to the specific anatomic injury or general surgical procedure performed.
Such patients are potentially unstable or have conditions that could pose a significant threat to life or risk of prolonged impairment. In order for these services to be paid, two reporting requirements must be met.
Critical Care Services Provided During Postoperative Period of Procedure With Global Period in Trauma and Burn Cases Postoperative critical care may be paid in addition to a global fee if the patient is critically ill and requires the constant attendance of the physician, and the critical care is unrelated to the specific anatomic injury or general surgical procedure performed.
No later than A. For further information refer to Medlearn Matters article number SE at www. For Survey and Certification requirements, a visit must occur no later than 30 days after admission.
This also applies to the NF with one exception. The only exception, as to who performs the initial visit, relates to the NF setting. Only a physician may report. The employer of the PA shall always report the visits performed by the PA.
Following the initial visit by the physician, payment shall be made for federally mandated visits that monitor and evaluate residents at least once every 30 days for the first 90 days after admission and at least once every 60 days thereafter.
Beginning January 1, , the new CPT code, Other Nursing Facility Service , may be used to report an annual nursing facility assessment visit on the required schedule of visits on an annual basis.
It shall not be performed in addition to the required number of federally mandated physician visits. Qualified NPPs, whether employed or not by the SNF, may perform alternating federally mandated physician visits, at the option of the physician, after the initial visit by the physician in a SNF.
Qualified NPPs in the NF setting, who are not employed by the NF, may perform federally mandated physician visits, at the option of the State, after the initial visit by the physician.
SNF Setting–Place of Service Code 31 Following the initial visit by the physician, the physician may delegate alternate federally mandated physician visits to a qualified NPP who meets collaboration and physician supervision requirements and is licensed as such by the State and performing within the scope of practice in that State.
Questions pertaining to writing orders or certification and recertification issues in the SNF and NF settings shall be addressed to the appropriate State Survey and Certification Agency departments for clarification.
The physician and the qualified NPP must be in the same group practice or be employed by the same employer. The Discharge Day Management Service may be reported using CPT code or , depending on the code requirement, for a patient who has expired, but only if the physician or qualified NPP personally performed the death pronouncement.
Assisted living facilities may also be known as adult living facilities. The Home Services codes should not be used for these places of service. Requirement for Physician Presence Home services codes are paid when they are billed to report evaluation and management services provided in a private residence.
A home visit cannot be billed by a physician unless the physician was actually present in the beneficiary’s home. Homebound Status Under the home health benefit the beneficiary must be confined to the home for services to be covered.
For home services provided by a physician using these codes, the beneficiary does not need to be confined to the home. The medical record must document the medical necessity of the home visit made in lieu of an office or outpatient visit.
Fee Schedule Payment for Services to Homebound Patients under General Supervision Payment may be made in some medically underserved areas where there is a lack of medical personnel and home health services for injections, EKGs, and venipunctures that.
Section 10 provides additional information on the provision of services to homebound Medicare patients. Required Companion Codes Prolonged services codes through are payable when they are billed on the same day by the same physician as the companion evaluation and management codes and: Prolonged services codes – are not paid unless they are accompanied by one of these companion codes.
Requirement for Physician Presence Physicians may count only the duration of direct face-to-face contact between the physician and the patient whether the service was continuous or not beyond the typical time of the visit code billed to determine whether prolonged services can be billed and to determine the prolonged services codes that are allowable.
In the case of prolonged office services, time spent by office staff with the patient, or time the patient remains unaccompanied in the office cannot be billed. In the case of prolonged hospital services, time spent waiting for test results, for changes in the patient’s condition, for end of a therapy, or for use of facilities cannot be billed as prolonged services.
Documentation Documentation is not required to accompany the bill for prolonged services unless the physician has been selected for medical review. Documentation is required in the medical record about the duration and content of the evaluation and management code billed and to show that the physician personally furnished the time specified in the HCPCS code definition.
Use of the Codes Prolonged services codes can be billed only if the total duration of all physician direct face-to-face service including the visit equals or exceeds the threshold time for the evaluation and management service the physician provided typical time plus 30 minutes.
If the total duration of direct face-to-face time does not equal or exceed the threshold time for the level of evaluation and management service the physician provided, the physician may not bill for prolonged services.
Threshold Times for Codes and If the total direct face-to-face time equals or exceeds the threshold time for code , but is less than the threshold time for code , the physician should bill the visit and code No more than one unit of is acceptable.
If the total direct face-toface time equals or exceeds the threshold time for code by no more than 29 minutes, the physician should bill the visit code and 1 unit of code One additional unit of code is billed for each additional increment of 30 minutes extended duration.
Add 30 minutes to the threshold time for billing codes and to get the threshold time for billing code and 2 units of code For example, to bill code and 2 units of code when billing a code , the threshold time is minutes.
Carriers do not accept more than 1 unit of code If the total direct face-to-face time equals or exceeds the threshold time for code by no more than 29 minutes, the physician bills the visit code and one unit of code Threshold Time to Bill Codes and 90 95 85 95 90 Carriers must add 30 minutes to the threshold time for billing codes and to get the threshold time for billing code and 2 units of A physician performed a visit that met the definition of visit code and the total duration of the direct face-to-face services including the visit was 65 minutes.
The physician bills code and 1 unit of code EXAMPLE 2 A physician performed a visit that met the definition of visit code and the total duration of the direct face-to-face contact including the visit was minutes.
The physician bills codes , , and 1 unit of code Examples of Nonbillable Prolonged Services EXAMPLE 1 A physician performed a visit that met the definition of visit code and the total duration of the direct face-to-face contact including the visit was 35 minutes.
The physician cannot bill prolonged services because the total duration of direct face-to-face service did not meet the threshold time for billing prolonged services.
EXAMPLE 2 A physician performed a visit that met the definition of code and, while the patient was in the office receiving treatment for 4 hours, the total duration of the direct face-toface service of the physician was 40 minutes.
Payment for these services is included in the payment for direct face-to-face services that physicians bill. The physician cannot bill the patient for these services since they are Medicare covered services and payment is included in the payment for other billable services.
Physicians may not bill Medicare or beneficiaries for standby services. Payment for standby services is included in the Part A payment to the facility. Such services are a part of hospital costs to provide quality care.
If hospitals pay physicians for standby services, such services are part of hospital costs to provide quality care. This section of the MMA states that payment for.
Due to the MMA requirement that the physician or treating practitioner create a written prescription and a regulatory requirement that the physician or treating practitioner prepare pertinent parts of the medical record for submission to the durable medical equipment supplier, code G physician service required to establish and document the need for a power mobility device has been established to recognize additional physician services and resources required to establish and document the need for the PMD.
The G code indicates that all of the information necessary to document the PMD prescription is included in the medical record, and the prescription and supporting documentation is delivered to the PMD supplier within 30 days after the face-to-face examination.
Effective October 25, , G will be used to recognize additional physician services and resources required to establish and document the need for the PMD and will be added to the Medicare physician fee schedule.
Team Conferences Team conferences codes may not be paid separately. Payment for these services is included in the payment for the services to which they relate.
Telephone Calls Telephone calls codes may not be paid separately. Payment for telephone calls is included in payment for billable services e. The national global surgery policy became effective for surgeries performed on and after January 1, The instructions that follow describe the components of a global surgical package and payment rules for minor surgeries, endoscopies and global surgical packages that are split.
In addition, billing, mandatory edits, claims review, adjudication, and postpayment instructions are included. In addition to the global policy, uniform payment policies and claims processing requirements have been established for other surgical issues, including bilateral and multiple surgeries, co-surgeons, and team surgeries.
The payment rules for surgical procedures apply to codes with entries of , , , and, sometimes, YYY. Payment is made for both the primary and the add-on codes, and the global period assigned is applied to the primary code.
Components of a Global Surgical Package Rev. The Medicare approved amount for these procedures includes payment for the following services related to the surgery when furnished by the physician who performs the surgery.
The services included in the global surgical package may be furnished in any setting, e. Visits to a patient in an intensive care or critical care unit are also included if made by the surgeon.
However, critical care services and are payable separately in some situations. Complications Following Surgery – All additional medical or surgical services required of the surgeon during the postoperative period of the surgery because of complications which do not require additional trips to the operating room; Postoperative Visits – Follow-up visits during the postoperative period of the surgery that are related to recovery from the surgery; Postsurgical Pain Management – By the surgeon; Supplies – Except for those identified as exclusions; and Miscellaneous Services – Items such as dressing changes; local incisional care; removal of operative pack; removal of cutaneous sutures and staples, lines, wires, tubes, drains, casts, and splints; insertion, irrigation and removal of urinary catheters, routine peripheral intravenous lines, nasogastric and rectal tubes; and changes and removal of tracheostomy tubes.
These services may be paid for separately. Please note that this policy only applies to major surgical procedures. The initial evaluation is always included in the allowance for a minor surgical procedure; Services of other physicians except where the surgeon and the other physician s agree on the transfer of care.
This agreement may be in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record; Visits unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery; Treatment for the underlying condition or an added course of treatment which is not part of normal recovery from surgery; Diagnostic tests and procedures, including diagnostic radiological procedures; Clearly distinct surgical procedures during the postoperative period which are not re-operations or treatment for complications.
A new postoperative period begins with the subsequent procedure. This includes procedures done in two or more parts for which the decision to stage the procedure is made prospectively or at the time of the first procedure.
Examples of this are procedures to diagnose and treat epilepsy codes , , , , and which may be performed in succession within 90 days of each other; Treatment for postoperative complications which requires a return trip to the operating room OR.
An OR for this purpose is defined as a place of service specifically equipped and staffed for the sole purpose of performing procedures. The term includes a cardiac catheterization suite, a laser suite, and an endoscopy suite.
It does not include a patient’s room, a minor treatment room, a recovery. This code is now a Status B and is no longer a separately payable service on or after January 1, However, splints and casting supplies are payable separately under the reasonable charge payment methodology; Immunosuppressive therapy for organ transplants; and Critical care services codes and unrelated to the surgery where a seriously injured or burned patient is critically ill and requires constant attendance of the physician.
Minor Surgeries and Endoscopies Visits by the same physician on the same day as a minor surgery or endoscopy are included in the payment for the procedure, unless a significant, separately identifiable service is also performed.
For example, a visit on the same day could be properly billed in addition to suturing a scalp wound if a full neurological examination is made for a patient with head trauma.
Billing for a visit would not be appropriate if the physician only identified the need for sutures and confirmed allergy and immunization status. A postoperative period of 10 days applies to some minor surgeries.
If the Field 16 entry is , carriers do not allow separate payment for postoperative visits or services within 10 days of the surgery that are related to recovery from the procedure.
If a diagnostic biopsy with a day global period precedes a major surgery on the same day or in the day period, the major surgery is payable separately. Services by other physicians are not included in the global fee for a minor procedures except as otherwise excluded.
If the Field 16 entry is , postoperative visits beyond the day of the procedure are not included in the payment amount for the surgery. Separate payment is made in this instance. Physicians Furnishing Less Than the Full Global Package B There are occasions when more than one physician provides services included in the global surgical package.
It may be the case that the physician who performs the surgical procedure does not furnish the follow-up care. Payment for the postoperative, postdischarge care is split between two or more physicians where the physicians agree on the transfer of care.
When more than one physician furnishes services that are included in the global surgical package, the sum of the amount approved for all physicians may not exceed what would have been paid if a single physician provides all services except where stated policies, e.
Where a transfer of care does not occur, the services of another physician may either be paid separately or denied for medical necessity reasons, depending on the circumstances of the case.
Determining the Duration of a Global Period To determine the global period for major surgeries, carriers count 1 day immediately before the day of surgery, the day of surgery, and the 90 days immediately following the day of surgery.
Date of surgery – January 5 Preoperative period – January 4 Last day of postoperative period – April 5 To determine the global period for minor procedures, carriers count the day of surgery and the appropriate number of days immediately following the date of surgery.
Procedure with 10 follow-up days: Date of surgery – January 5 Last day of postoperative period – January Physicians Who Furnish the Entire Global Surgical Package Physicians who perform the surgery and furnish all of the usual pre-and postoperative work bill for the global package by entering the appropriate CPT code for the surgical procedure only.
Billing is not allowed for visits or other services that are included in the global package. Physicians in Group Practice When different physicians in a group practice participate in the care of the patient, the group bills for the entire global package if the physicians reassign benefits to the group.
The physician who performs the surgery is shown as the performing physician. Physicians Who Furnish Part of a Global Surgical Package Where physicians agree on the transfer of care during the global period, the following modifiers are used: Both the bill for the surgical care only and the bill for the postoperative care only, will contain the same date of service and the same surgical procedure code, with the services distinguished by the use of the appropriate modifier.
Providers need not specify on the claim that care has been transferred. However, the date on which care was relinquished or assumed, as applicable, must be shown on the claim.
Both the surgeon and the physician providing the postoperative care must keep a copy of the written transfer agreement in the beneficiary’s medical record. No modifiers are necessary on the claim.
Physicians who provide follow-up services for minor procedures performed in emergency departments bill the appropriate level of office visit code. The physician who performs the emergency room service bills for the surgical procedure without a modifier.
If the services of a physician other than the surgeon are required during a postoperative period for an underlying condition or medical complication, the other physician reports the appropriate evaluation and management code.
An example is a cardiologist who manages underlying cardiovascular conditions of a patient. Evaluation and management services on the day before major surgery or on the day of major surgery that result in the initial decision to perform the surgery are not included in the global surgery payment for the major surgery and, therefore, may be billed and paid separately.
Moreover, where the decision to perform the minor procedure is typically done immediately before the service, it is considered a routine preoperative service and a visit or consultation is not billed in addition to the procedure.
Return Trips to the Operating Room During the Postoperative Period When treatment for complications requires a return trip to the operating room, physicians must bill the CPT code that describes the procedure s performed during the return trip.
If no such code exists, use the unspecified procedure code in the correct series, i. The procedure code for the original surgery is not used except when the identical procedure is repeated.
The physician may also need to indicate that another procedure was performed during the postoperative period of the initial procedure. The CPT definition for this modifier does not limit its use to treatment for complications.
This modifier is not used to report the treatment of a problem that requires a return to the operating room. The physician may need to indicate that the performance of a procedure or service during the postoperative period was: Planned prospectively or at the time of the original procedure; b.
More extensive than the original procedure; or c. For therapy following a diagnostic surgical procedure. A new postoperative period begins when the next procedure in the series is billed.
Unrelated Procedures or Visits During the Postoperative Period Two CPT modifiers were established to simplify billing for visits and other procedures which are furnished during the postoperative period of a surgical procedure, but which are not included in the payment for the surgical procedure.
Reports an unrelated procedure by the same physician during a postoperative period. The physician may need to indicate that the performance of a procedure or service during a postoperative period was unrelated to the original procedure.
A new postoperative period begins when the unrelated procedure is billed. Reports an unrelated evaluation and management service by same physician during a postoperative period.
The physician may need to indicate that an evaluation and management service was performed during the postoperative period of an unrelated procedure. An ICDCM code that clearly indicates that the reason for the encounter was unrelated to the surgery is acceptable documentation.
It is used to report a significant, separately identifiable evaluation and management service by same physician on the day of a procedure. The physician may need to indicate that on the day a procedure or service that is identified with a CPT code was performed, the patient’s condition required a significant, separately identifiable evaluation and management service above and beyond the usual preoperative and postoperative care associated with the procedure or service that was performed.
Critical Care Critical care services provided during a global surgical period for a seriously injured or burned patient are not considered related to a surgical procedure and may be paid separately under the following circumstances.
Preoperative and postoperative critical care may be paid in addition to a global fee if: In order for these services to be paid, two reporting requirements must be met: The biller must provide: Date s of Service.
This will enable carriers to relate all appropriate billings to the correct surgery. Physicians who share postoperative management with another physician must submit additional information showing when they assumed and relinquished responsibility for the postoperative care.
The physician providing the remaining postoperative care must show the date care was assumed. Care Provided in Different Payment Localities If portions of the global period are provided in different payment localities, the services should be billed to the carriers servicing each applicable payment locality.
The following are guidelines for the appropriate billing procedures: The 10 percent bonus will be paid on the appropriate postoperative portion only. If a claim is submitted with a global surgical code and a HPSA modifier, the carrier assumes that the entire global service was provided in a HPSA in the absence of evidence otherwise.
The sum of the payments made for the surgical and postoperative services provided in different localities will not equal the global amount in either of the localities because of geographic adjustments made through the Geographic Practice Cost Indices.
Relationship to Correct Coding Initiative CCI The CCI policy and computer edits allow carriers to detect instances of fragmented billing for certain intra-operative services and other services furnished on the same day as the surgery that are considered to be components of the surgical procedure and, therefore, included in the global surgical fee.
When both correct coding and global surgery edits apply to the same claim, carriers first apply the correct coding edits, then, apply the global surgery edits to the correctly coded services. Prepayment Edits to Detect Separate Billing of Services Included in the Global Package In addition to the correct coding edits, carriers must be capable of detecting certain other services included in the payment for a major or minor surgery or for an endoscopy.
On a prepayment basis, carriers identify the services that meet the following conditions: Carriers use the following evaluation and management codes in establishing edits for visits included in the global package.
CPT codes , , , , , , , , , , , , , , and have been transferred from the excluded category and are now included in the global surgery edits. Evaluation and Management Codes for Carrier Edits


